New Urothelial carcinoma treatments 2024
New Urothelial carcinoma Treatments 2024
Urothelial carcinoma, also known as transitional cell carcinoma, is a type of cancer that occurs in the urothelial cells lining the inside of the bladder and can also affect other parts of the urinary tract such as the ureters, urethra, and kidneys. It is the most common form of bladder cancer and is characterized by its tendency to recur after treatment, necessitating ongoing surveillance. Risk factors for developing urothelial carcinoma include smoking, exposure to certain chemicals, chronic bladder inflammation, and a history of radiation therapy. Symptoms often include blood in the urine (hematuria), frequent urination, pain during urination, and pelvic pain. Early detection is crucial for effective treatment, which may involve surgery, chemotherapy, radiation, or immunotherapy, depending on the stage and grade of the cancer.
When considering treatment options for urothelial carcinoma, it is important to consult with a healthcare professional to understand the specific characteristics of the disease and to discuss the benefits and risks of each treatment. Surgery is often the first-line treatment, especially for non-muscle invasive bladder cancer, and may range from transurethral resection to more extensive procedures like cystectomy. Intravesical therapy, where medicine is placed directly into the bladder, is another option for early-stage disease. For advanced or metastatic urothelial carcinoma, systemic chemotherapy, immunotherapy agents like checkpoint inhibitors, or targeted therapies may be recommended. Clinical trials may also be an option for patients seeking access to cutting-edge treatments that are not yet widely available.
Treatment options
| Treatment option | Estimated cost | Efficacy | Eligibility |
|---|---|---|---|
| Surgery (Transurethral resection, Cystectomy) | Varies widely | Can be curative for early-stage cancers | Typically for localized tumors |
| Chemotherapy (Cisplatin, Gemcitabine) | $1,000 - $5,000 | Varies; cisplatin unsuitable for patients with poor renal function | Widely used; some patients ineligible for cisplatin |
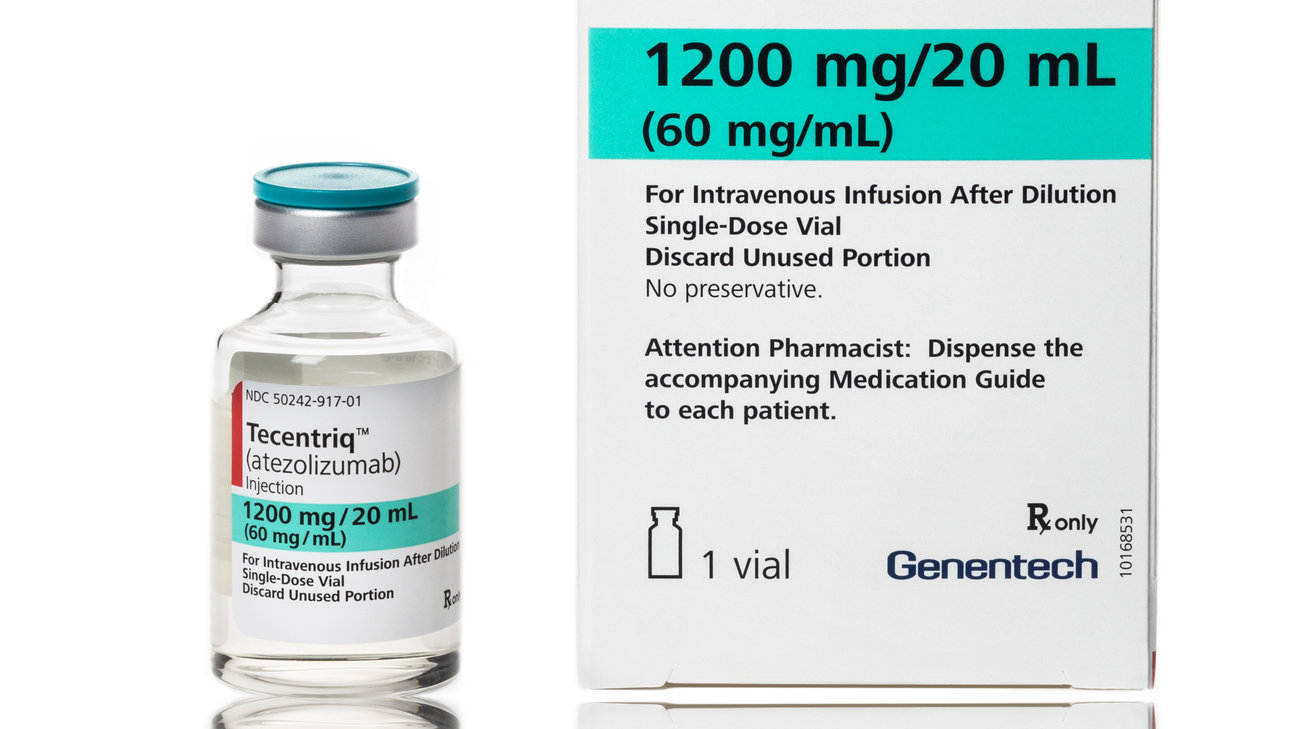
| Immunotherapy (Tecentriq) | $13,000 - $16,000 | Improved survival in metastatic setting | FDA-approved for locally advanced or metastatic urothelial carcinoma |
| Immunotherapy (Opdivo) | $13,000 - $16,000 | Shown to be effective in metastatic or surgically unresectable urothelial carcinoma | FDA-approved for patients who have disease progression during or following platinum-containing chemotherapy |
| Immunotherapy (Keytruda) | $13,000 - $16,000 | Improves overall survival in some patients | FDA-approved for locally advanced or metastatic urothelial carcinoma |
| Immunotherapy (Imfinzi) | $13,000 - $16,000 | Shown to delay progression after chemotherapy | FDA-approved for locally advanced or metastatic urothelial carcinoma |
| Immunotherapy (Bavencio) | $13,000 - $16,000 | Can lead to durable responses | FDA-approved for locally advanced or metastatic urothelial carcinoma |
| Antibody-drug conjugate (Trodelvy) | $18,000 - $20,000 | Shows activity in metastatic disease | For patients who have previously received a platinum-containing chemotherapy and either a PD-1 or PD-L1 inhibitor |
| Antibody-drug conjugate (Padcev) | $18,000 - $20,000 | Effective in some patients with advanced disease | FDA-approved for locally advanced or metastatic urothelial cancer who have previously received a PD-1 or PD-L1 inhibitor and a platinum-containing chemotherapy |
| Radiation therapy | $2,000 - $10,000 | Can be curative in combination with chemotherapy for localized disease | Typically for localized tumors or for palliation |
| Experimental treatments (Clinical trials) | Costs may be covered by the trial sponsor | Varies; not yet proven | Eligibility depends on specific trial criteria |
Treatments options in detail
First-Line Treatment for Urothelial Carcinoma
The most common first-line treatment for urothelial carcinoma, particularly for muscle-invasive and metastatic disease, is cisplatin-based chemotherapy. The regimen often includes a combination of cisplatin with gemcitabine. For patients who are ineligible for cisplatin due to poor kidney function or other health issues, carboplatin may be used as an alternative, though it is generally considered less effective.
Immunotherapy Agents
Immunotherapy has become a cornerstone in the management of urothelial carcinoma, especially for patients who cannot tolerate or have progressed after cisplatin-based chemotherapy. Atezolizumab (Tecentriq) and pembrolizumab (Keytruda) are programmed death-ligand 1 (PD-L1) inhibitors approved by the FDA for first-line treatment in cisplatin-ineligible patients and as second-line therapy after chemotherapy failure. Nivolumab (Opdivo) is another PD-1 inhibitor approved for use after chemotherapy in metastatic urothelial carcinoma.
Durvalumab (Imfinzi), an anti-PD-L1 agent, and avelumab (Bavencio), an anti-PD-L1 antibody, are also approved for use in patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
Targeted Therapy
Erdafitinib (Balversa) is a targeted therapy approved for the treatment of urothelial carcinoma. It is a fibroblast growth factor receptor (FGFR) inhibitor used in patients with susceptible FGFR3 or FGFR2 genetic alterations and who have progressed during or following at least one line of prior platinum-containing chemotherapy, including within 12 months of neoadjuvant or adjuvant chemotherapy.
Antibody-Drug Conjugates
Enfortumab vedotin (Padcev) is an antibody-drug conjugate targeting Nectin-4, a protein found on the surface of most urothelial cancer cells. It is approved for patients who have previously received a PD-1 or PD-L1 inhibitor and a platinum-containing chemotherapy in the neoadjuvant/adjuvant, locally advanced or metastatic setting.
Sacituzumab govitecan (Trodelvy) is another antibody-drug conjugate that has shown promise in the treatment of metastatic urothelial cancer. It targets Trop-2, a protein expressed on many types of cancer cells, including urothelial carcinoma. While not yet approved by the FDA specifically for urothelial carcinoma, it has been granted accelerated approval for metastatic triple-negative breast cancer and is being studied in urothelial carcinoma clinical trials.
Radiation Therapy
Radiation therapy may be used as a primary treatment for patients who are not candidates for surgery or in combination with chemotherapy for muscle-invasive bladder cancer. It can also be used as a palliative treatment to relieve symptoms in cases of advanced disease.
Surgery
Surgical options for urothelial carcinoma include transurethral resection of bladder tumor (TURBT) for non-muscle invasive bladder cancer, partial cystectomy, and radical cystectomy with urinary diversion for muscle-invasive disease. In select cases of upper tract urothelial carcinoma, nephroureterectomy with removal of the bladder cuff is the standard treatment.
Chemotherapy for Non-Muscle Invasive Disease
Intravesical therapy with agents such as Bacillus Calmette-Guérin (BCG) or mitomycin C is commonly used for non-muscle invasive bladder cancer following TURBT. BCG is considered the most effective intravesical immunotherapy for preventing recurrence and progression of high-grade non-muscle invasive bladder cancer.
Experimental Treatments
Experimental treatments for urothelial carcinoma include novel immunotherapies, targeted therapies, and combination regimens that are currently being evaluated in clinical trials. These include new checkpoint inhibitors, antibody-drug conjugates, and FGFR inhibitors, among others. The use of these agents is based on the evolving understanding of the molecular biology of urothelial carcinoma and the tumor microenvironment.
Treatments Not Approved by the FDA
Treatments not approved by the FDA for urothelial carcinoma but used in clinical practice include off-label use of chemotherapeutic agents and targeted therapies based on the molecular profiling of individual tumors. Physicians may choose to use these treatments in a compassionate use scenario or as part of a clinical trial. It is important for patients to discuss the potential risks and benefits of such treatments with their healthcare provider.
Conclusion
The treatment landscape for urothelial carcinoma is rapidly evolving with the introduction of new therapies and the application of personalized medicine. As research continues and more therapies are tested in clinical trials, the options for patients with urothelial carcinoma are expected to expand, offering hope for improved outcomes and quality of life.
Symptoms
Symptoms of Urothelial Carcinoma
Urothelial carcinoma, also known as transitional cell carcinoma, primarily affects the urinary system, including the bladder, ureters, and renal pelvis. The most common symptom associated with urothelial carcinoma is hematuria, which is blood in the urine. This symptom is often painless and can be visible to the naked eye (gross hematuria) or detectable only under a microscope (microscopic hematuria).
Another frequent symptom is dysuria, which is pain or discomfort during urination. Patients may experience a burning sensation or a feeling of urgency and frequency when they need to urinate. These urinary symptoms are not specific to urothelial carcinoma and can be associated with other conditions such as urinary tract infections or benign prostatic hyperplasia.
Individuals with urothelial carcinoma may also report changes in urinary habits, including the need to urinate more frequently than usual, especially at night (nocturia), or the sudden, strong desire to urinate that is hard to control (urgency).
In some cases, patients may experience pelvic or back pain, which can be indicative of advanced disease or the tumor's invasion into surrounding tissues. The pain can be persistent or intermittent and may vary in intensity.
Another symptom that may be present is a palpable mass in the pelvic area, although this is less common and typically occurs in more advanced stages of the disease.
Urothelial carcinoma can also lead to urinary tract obstruction, which can manifest as difficulty urinating or a weak urine stream. In more severe cases, complete urinary blockage can occur, leading to complications such as kidney damage or infection.
Weight loss, fatigue, and a general feeling of being unwell (malaise) are nonspecific symptoms that can also be associated with urothelial carcinoma, especially in more advanced stages of the disease.
Less commonly, individuals with urothelial carcinoma may experience symptoms related to metastasis, which is the spread of cancer to other parts of the body. These symptoms depend on the location of the metastasis and can include bone pain, cough or shortness of breath if the lungs are involved, or neurological symptoms if the cancer has spread to the brain or spinal cord.
It is important to note that the presence of these symptoms does not necessarily mean that an individual has urothelial carcinoma, as they can be caused by a variety of other conditions. A thorough evaluation by a healthcare professional, including diagnostic tests, is required to determine the cause of these symptoms.
Early detection and diagnosis are crucial for the effective management of urothelial carcinoma. Individuals experiencing any of the above symptoms, especially hematuria, should seek medical attention promptly for evaluation and appropriate diagnostic testing.
Cure
Current Therapeutic Approaches to Urothelial Carcinoma
Urothelial carcinoma, particularly when detected at an early stage, can often be managed effectively with a combination of treatments. However, the term 'cure' implies the complete eradication of cancer with no chance of recurrence, which is a scenario that is not guaranteed with any current treatment for urothelial carcinoma. The term 'cure' is thus used cautiously by medical professionals, and the focus is often on treatment, management, and remission.
Surgical Interventions
Surgery is the primary treatment for localized urothelial carcinoma and can be curative in many cases of non-muscle-invasive bladder cancer (NMIBC). Transurethral resection of bladder tumor (TURBT) is the standard initial treatment for NMIBC. For muscle-invasive bladder cancer (MIBC), radical cystectomy, which involves the removal of the entire bladder and surrounding lymph nodes, may be performed. In some cases, a neobladder reconstruction can be done, allowing for a more normal urinary function post-surgery. The success of surgical interventions as a curative approach depends on the stage and grade of the tumor, as well as the presence of any metastases.
Intravesical Therapy
Following TURBT, intravesical therapy, which involves the direct instillation of immunotherapy or chemotherapy into the bladder, is used to reduce the risk of recurrence and progression of NMIBC. Bacillus Calmette-Guérin (BCG) therapy is the most effective intravesical immunotherapy for NMIBC and has been shown to be curative in some cases. Intravesical chemotherapy agents, such as mitomycin C and thiotepa, are also used, particularly for patients who are not candidates for BCG therapy.
Systemic Chemotherapy
For patients with MIBC or metastatic urothelial carcinoma, systemic chemotherapy is a standard treatment option. Neoadjuvant chemotherapy, given before surgery, can improve survival and may lead to a cure in a subset of patients by eradicating micrometastatic disease. Adjuvant chemotherapy, given after surgery, may also be recommended in cases where there is a high risk of recurrence. Platinum-based chemotherapy regimens, such as MVAC (methotrexate, vinblastine, doxorubicin, and cisplatin) or gemcitabine and cisplatin, are commonly used. However, not all patients are cured with chemotherapy, and the potential for recurrence remains.
Immunotherapy
Recent advances have introduced immune checkpoint inhibitors as a new treatment modality for urothelial carcinoma. Agents such as pembrolizumab, atezolizumab, nivolumab, and durvalumab have been approved for use in patients with locally advanced or metastatic urothelial carcinoma who are not candidates for cisplatin-containing chemotherapy or who have progressed on or after platinum-based chemotherapy. These agents work by enhancing the body's immune response against cancer cells. While durable responses and prolonged survival have been observed in a subset of patients, these treatments do not guarantee a cure and are associated with a unique set of immune-related side effects.
Targeted Therapy
Targeted therapy represents another approach to the treatment of urothelial carcinoma. Drugs such as erdafitinib target specific genetic alterations in tumor cells, such as mutations in the FGFR3 gene. These therapies can lead to significant tumor shrinkage and prolonged disease control in selected patients. However, targeted therapies are not considered curative and are generally used for disease management, particularly in the metastatic setting.
Radiation Therapy
Radiation therapy is sometimes used as part of a bladder-preserving approach in combination with chemotherapy for muscle-invasive disease or as a definitive treatment in patients who are not surgical candidates. While radiation therapy can be effective in controlling local disease and may contribute to long-term survival, it is not typically considered a curative treatment on its own for urothelial carcinoma.
Prospects of a Cure
The possibility of curing urothelial carcinoma is influenced by various factors, including the stage at diagnosis, tumor grade, response to treatment, and the presence of certain molecular characteristics within the tumor. Early-stage, low-grade tumors that are localized to the bladder lining have the best prognosis and the highest potential for cure, especially when treated promptly and appropriately. However, urothelial carcinoma, especially in advanced stages, carries a risk of recurrence and progression, which can complicate the achievement of a definitive cure.
Follow-up and Surveillance
Due to the risk of recurrence and progression, patients treated for urothelial carcinoma require long-term follow-up and surveillance. This typically includes regular cystoscopies, imaging studies, and urine cytology. Surveillance is critical to detect recurrences early when they may be more amenable to curative treatment. The intensity of surveillance depends on the initial stage and grade of the tumor, as well as the treatments received.
Conclusion
In summary, while there is no guaranteed cure for urothelial carcinoma, there are multiple treatment strategies that can lead to remission and potentially long-term disease-free survival, particularly for early-stage disease. The concept of a cure in the context of urothelial carcinoma is complex and is best understood in terms of probability rather than certainty. Treatment decisions are highly individualized and depend on a multitude of factors, including the patient's overall health, preferences, and the specific characteristics of their cancer.
Access Urothelial carcinoma medicines today
If Urothelial carcinoma medicines are not approved or available in your country (e.g. due to supply issues), you can access them via Everyone.org.
How Everyone.org works

Make an enquiry
Choose the medicine you want to access, answer a couple of questions, and upload your prescription to speed things up. We’ll get back to you within 24 hours.


Make an enquiry
Choose the medicine you want to access, answer a couple of questions, and upload your prescription to speed things up. We’ll get back to you within 24 hours.


Breeze through the paperwork
We'll guide you through the required documents for importing unapproved medicine, ensuring you have all the necessary information.


Get a personalized quote
We’ll prepare a quote for you, including medicine costs and any shipping, administrative, or import fees that may apply.


Receive your medicine
Accept the quote and we’ll handle the rest - sourcing and safely delivering your medicine.

Some text on this page has been automatically generated. Speak to your physician before you start a new treatment or medication.
Let's talk
If you have any questions, call us or send us a message through WhatsApp or email:
Contact us